AUTONOMIC NERVOUS SYSTEM
DIVISIONS OF THE AUTONOMIC NERVOUS SYSTEM
SYMPATHETIC DIVISION PATHWAYS
The cell bodies of the preganglionic axons of the sympathetic division are located in segments T1 through L3 of the lateral horn of the spinal cord. From here, these axons project away from the spinal cord through the ventral root and enter a spinal nerve. They then exit the spinal nerve through a white ramus communicans (myelinated axons), and enter a sympathetic chain ganglia, which are ganglia located along the spinal cord bilaterally. The following are descriptions of four different routes taken by sympathetic axons traveling from the CNS, to their effectors (organs, glands, and vessels) (see figures below).
1. Preganglionic axons synapse at the sympathetic chain ganglia with a postganglionic neuron. The postganglionic neuron then leaves the sympathetic chain ganglia through a gray ramus communicans (unmyelinated axons) and reenters the spinal nerve and travels to the skin and blood vessels throughout the body.
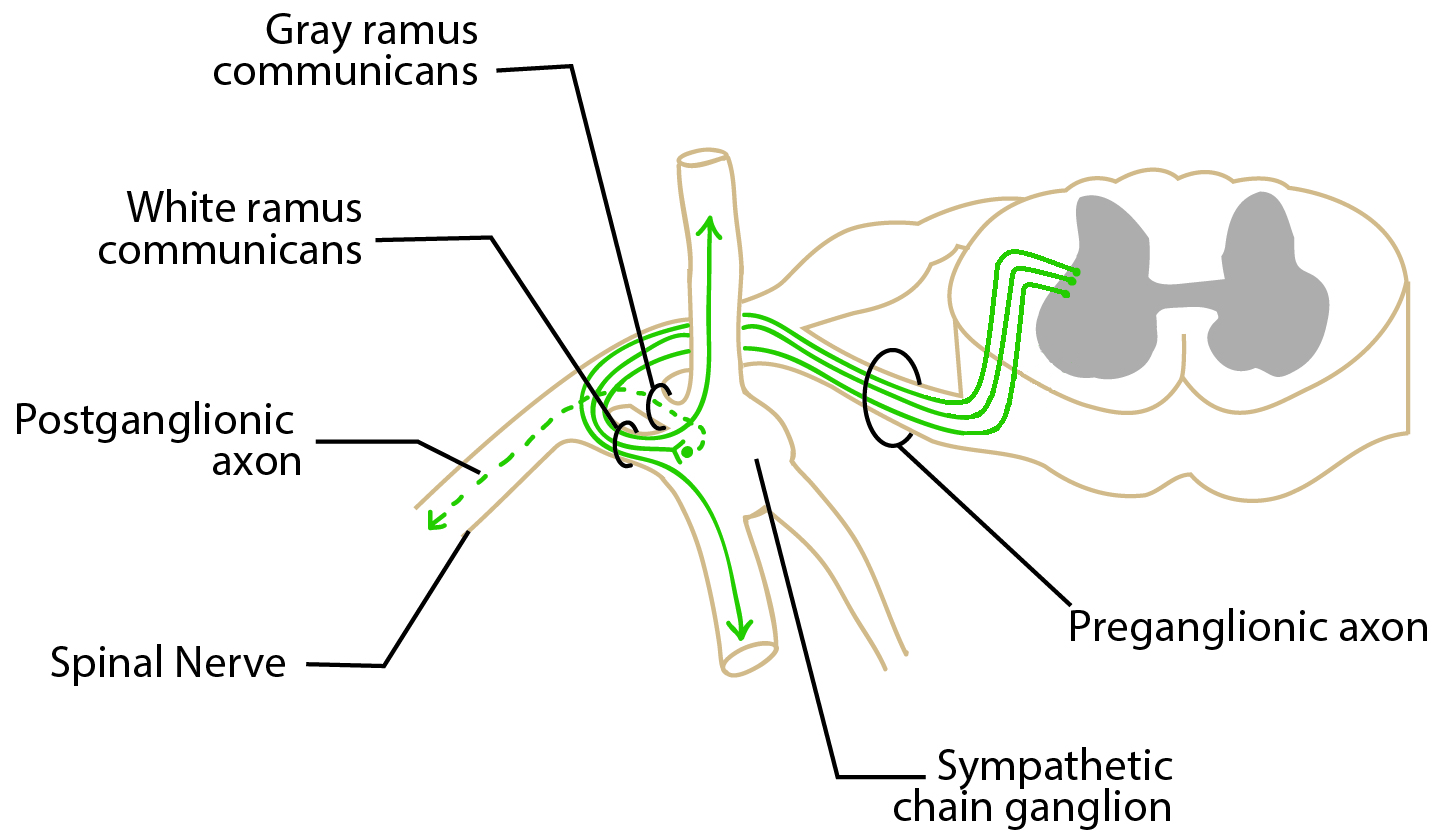
Image by BYU-I student, Kaylyn Lloyd Winter 2014
In the image above, preganglionic axons enter a sympathetic chain ganglion via a white ramus communicans (called white because the axons are myelinated which gives a more whitish appearance to this "bridge). Some axons synapse with postganglionic neurons in the sympathetic chain ganglion, while others travel to inferior or superior sympathetic chain ganglia before synapsing. Postganglionic axons leave sympathetic chain ganglia via a gray ramus communicans (called gray because the postganglionic neurons are not myelinated which gives a grayish appearance to the "bridge") and enter a spinal nerve. The spinal nerve carries the postganglionic axon out the peripheral body with other sensory and motor neurons.
2. The second type is very similar, but instead of the postganglionic neuron entering a spinal nerve, it enters a sympathetic nerve and travels to organs of the thoracic cavity. See below.
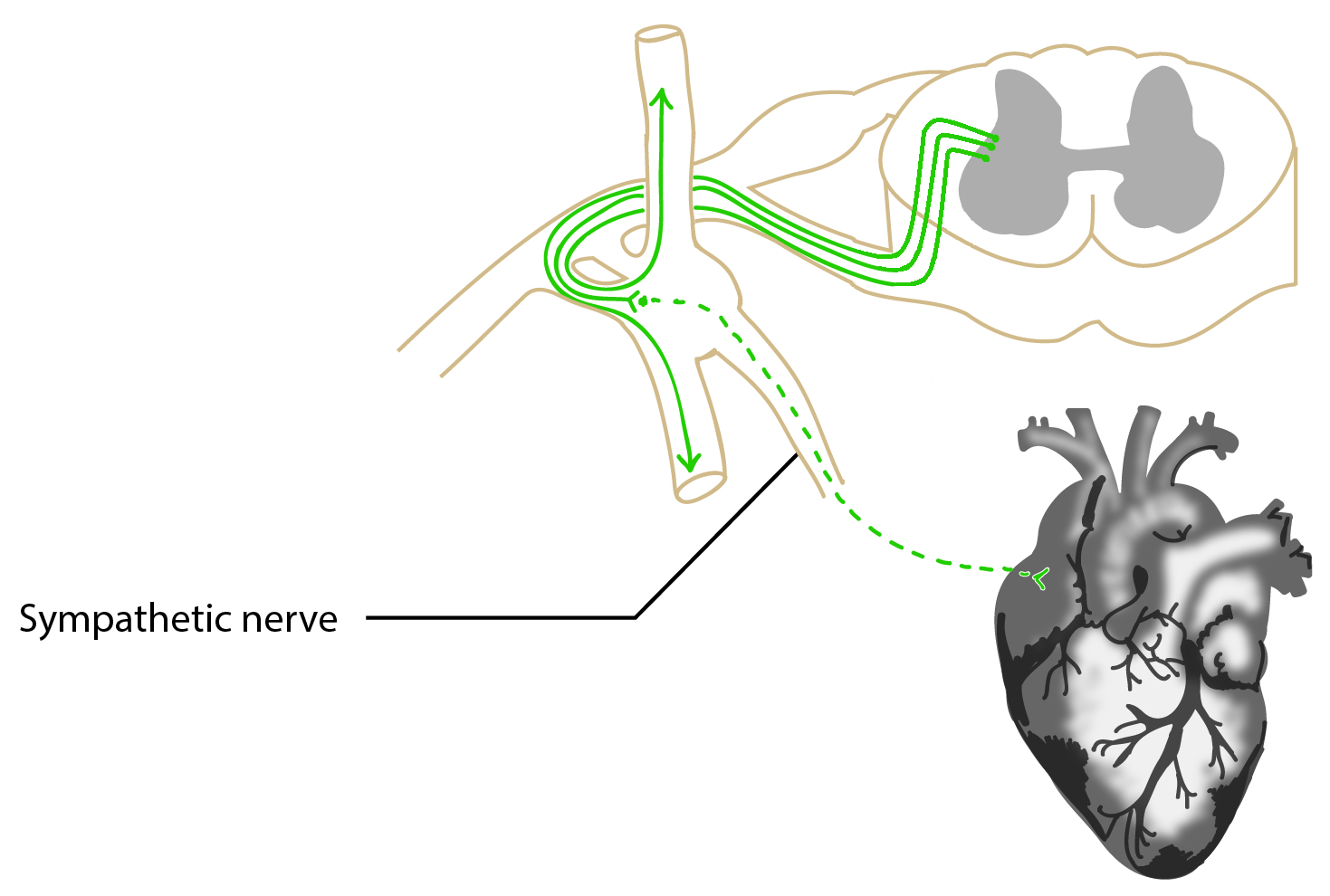
Image by BYU-I student, Kaylyn Lloyd Winter 2014
3. The preganglionic neuron enters and leaves the sympathetic chain ganglion without synapsing and forms a splanchnic nerve and travels to collateral ganglia. At these ganglia, the preganglionic neurons synapse with postganglionic neurons which then extend to organs, glands, and vessels of the abdominopelvic cavity. See below.
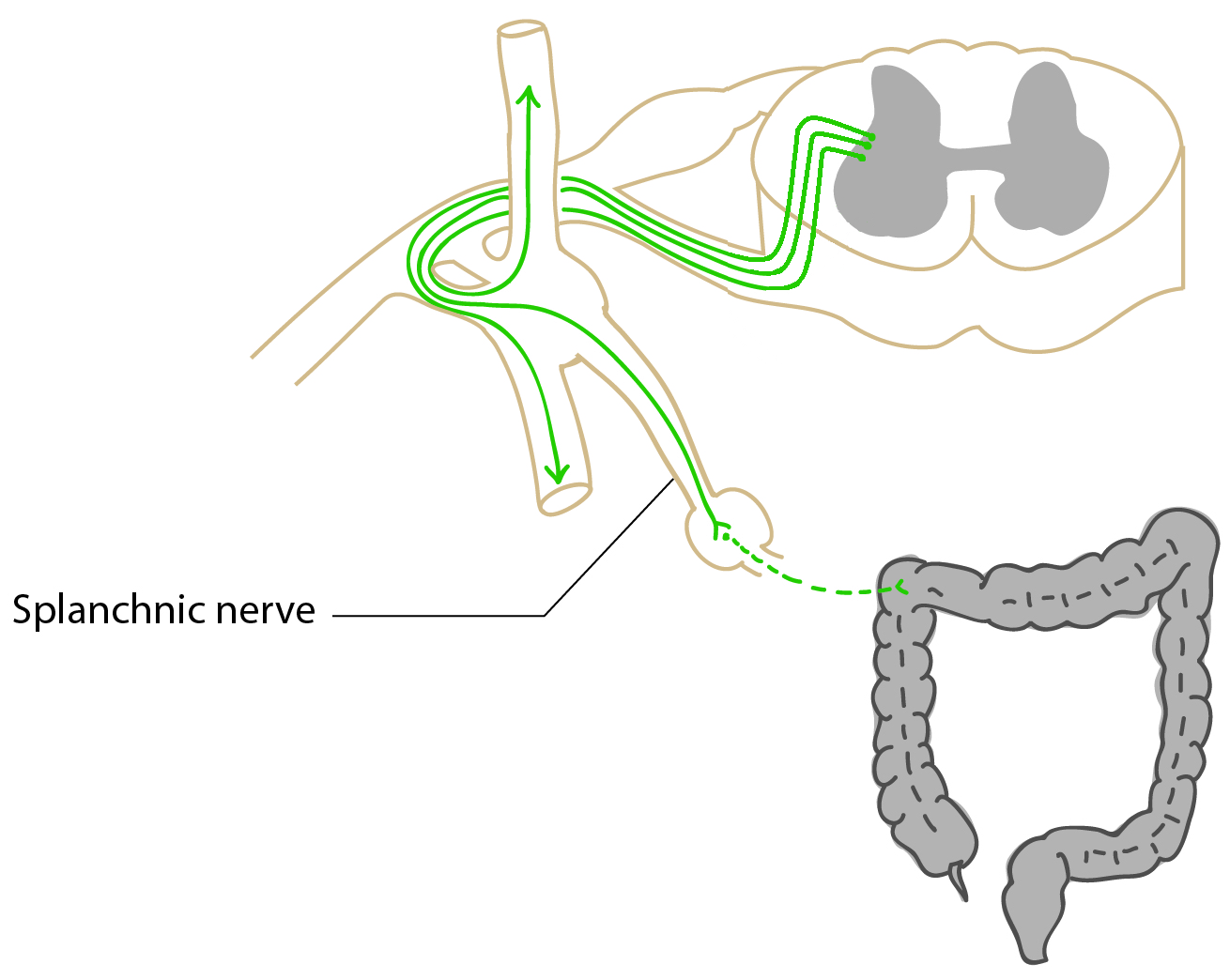
Image by BYU-I student, Kaylyn Lloyd Winter 2014
4. The last route for sympathetic axons is similar to those traveling through splanchnic nerves, but instead of synapsing, they travel straight through collateral ganglia. They then extend to the medulla of the adrenal gland, where they synapse with cells that produce epinephrine (EPI) and norepinephrine (NE). These medullary cells function as modified postganglionic neurons and release secretory product directly into the blood rather than into a synapse. About 80% of adrenal medullary cells produce EPI and the other 20% produce NE. After release into the blood, these hormones travel to receptors throughout the body to elicit a "fright, flight, or fright" response. See below.
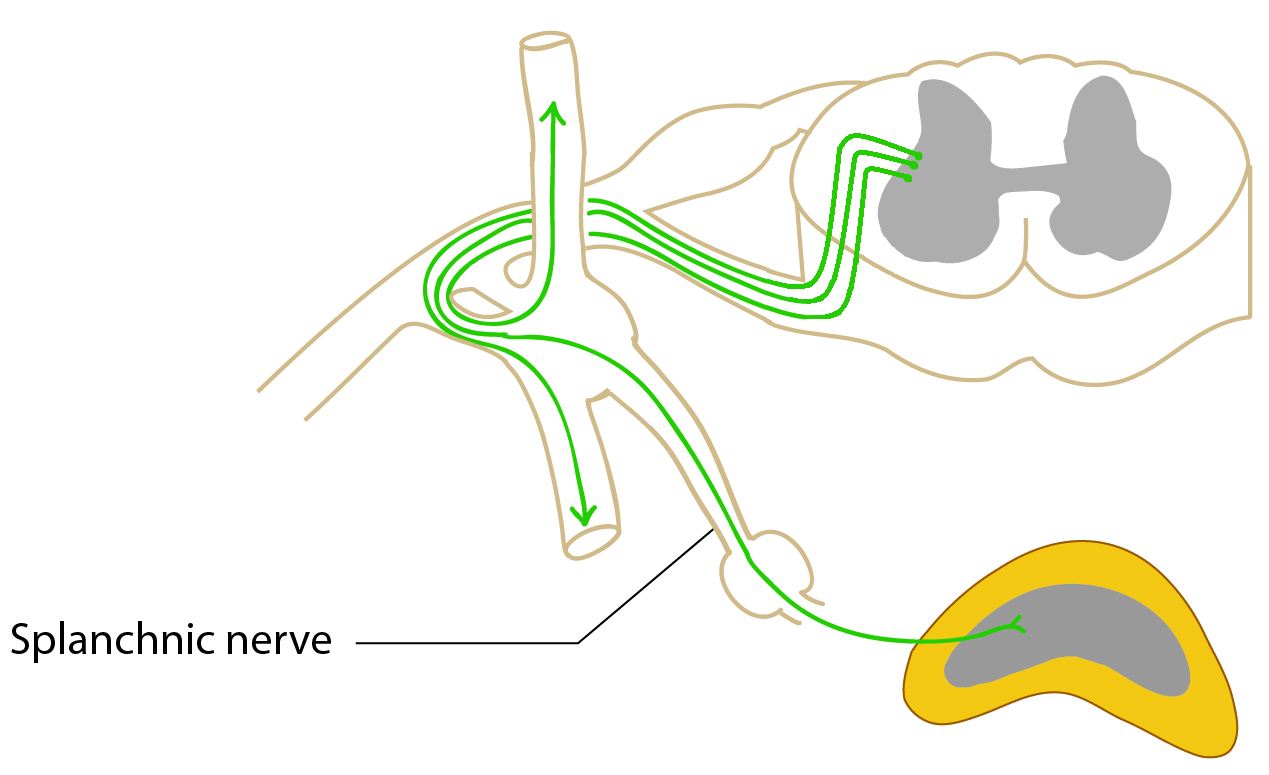
Image by BYU-I student, Kaylyn Lloyd Winter 2014
Click on this highlighted link to follow an image search that will show some more pictures for pathways of the sympathetic nervous system.
About 8% of the fibers in the 31 pairs of spinal nerves are postganglionic sympathetic fibers. Some of these fibers innervate the effectors of the skin-particularly capillaries and sweat glands. The sympathetic division also innervates the iris lens, nasal mucus membranes, salivary glands, the heart, lungs, stomach, intestines, adrenal gland, and urinary bladder (see figure below).
Parasympathetic Division
The parasympathetic division does not follow 4 pathways like the sympathetic division. The parasympathetic division sends preganglionic neurons from the cranial area and the sacral area. This is why it is also known as the craniosacral division.
Cranio: Preganglionic cell bodies for coming from the brain are located in the brainstem and make up part of the cell bodies of cranial nerves - namely, cranial nerves III (oculomotor) which control the size of the pupil and shape of the lens, VII (facial) which control nasal mucus membranes and lacrimal and salivary glands, IX (glossopharyngeal) which controls the parotid salivary gland, and the X (vagus) which innervates organs of the thoracic cavity and upper abdominal cavity including the lungs, heart, stomach, pancreas, small intestine, liver, and upper portion of the large intestine. The vagus nerve is the major nerve of the cranial parasympathetic division. 75-80% of all parasympathetic fibers are found in the vagus nerve.
Sacral: There are a few preganglionic neuron cell bodies of the parasympathetic division that are located in the sacral region of the lateral horn of the spinal cord. Axons from these neurons enter pelvic splanchnic nerves and then extend to terminal ganglia which are located near or on the effector. Effectors innervated by the lower portion of the parasympathetic nervous system include the lower half of the large intestine and organs of the reproductive and renal systems. It helps to have images of the ANS anatomy in hand as you study these ANS divisions.
You can click here to review the image of the SNS anatomy
You can click here to review the image of the PNS anatomy
Here is one more image (click here) that is excellent
Enteric Nervous System
The enteric nervous system (ENS) is sometimes referred to as the third division of the nervous system (central, peripheral, and enteric). This system is composed of a nerve plexus or a meshwork of fibers innervating the digestive tract from the esophagus to the distal colon. The ENS includes the myenteric plexus and the submucosal plexus which receive preganglionic fibers from the parasympathetic division and postganglionic fibers from the sympathetic division of the ANS. Innervation from the ANS and sensory input from within the wall of the gut work together to control smooth muscle motor activity and gut secretory actions. However, the ENS releases a variety of neurotransmitters and is capable of controlling digestive functions independently of the CNS by way of local reflexes. When food is introduced into the digestive tract, stretch receptors in the gut are activated and send action potentials through afferent enteric sensory neurons. These neurons synapse with entericinterneurons which are capable of activating efferent enteric motor neurons. These neurons innervate glands and smooth muscle. Their increased activity enhances digestive enzyme secretions and gut contraction to cause mixing and propulsion of food. The ENS is particularly important in providing synchronous peristaltic movements ensuring propulsion of food in one direction (see figure below).
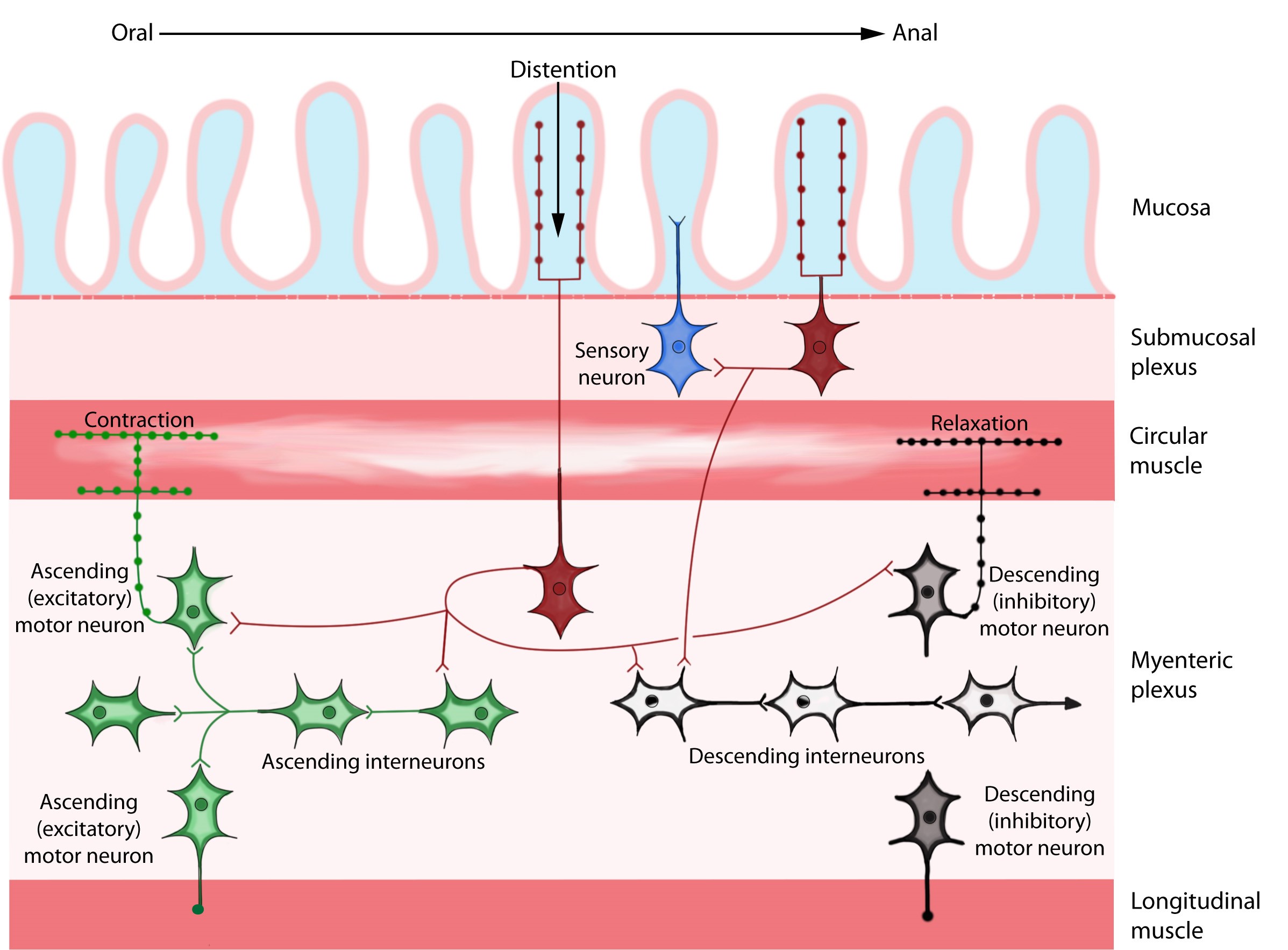
Image by BYU-I student 2014
The enteric nervous system, showing the submucosal and myenteric plexuses.
**You may use the buttons below to go to the next or previous reading in this Module**


