- Public
- Private
Healthcare Industry Sector 1: The Public Sector
Public Health Administration is focused on the provision of healthcare
services by the "government" —federal, state, county and
municipal. Healthcare policy is the domain of government agencies.
The U.S. Department of Health and Human Services (HHS) is a
cabinet-level department of the federal government. Alex Azar is
currently the Acting Secretary of HHS, sworn in on January 29, 2019.
Within the Department of Health and Human Services is the Division known as the Centers for Medicare and Medicaid Services [CMS], formerly known as HCFA—the Healthcare Financing Administration. CMS is the entity that is responsible for administering the Medicare program nationally, and playing a "coordinating" role with the individual states, who administer their respective Medicaid programs.
Given the nature of political appointments, it should be anticipated
that changes in this significant cabinet position will occur
periodically.
For the organizational chart of HHS, go to HHS.gov and there you will find a detailed organizational chart of the entire department.
Hospitals in the United States
| Total Number of All U.S. Hospitals | 6,146 |
| Number of U.S. Community Hospitals |
5,198 |
| Number of Non-government Not-for-Profit Community Hospitals |
2,937 |
| Number of Investor-Owned (For-Profit) Community Hospitals |
1,296 |
| Number of State and Local Government Community Hospitals |
965 |
| Number of Federal Government Hospitals |
209 |
| Number of Nonfederal Psychiatric Hospitals |
616 |
Source:
American Hospital Association, 2020
Definitions
- Registered Hospitals
- Registered hospitals are those hospitals that meet AHA's criteria for registration as a hospital facility. Registered hospitals include AHA member hospitals as well as nonmember hospitals. For a complete listing of the criteria used for registration, please see "AHA Registration Requirements for Hospitals."
- Community Hospitals
- Community hospitals are defined as all nonfederal, short-term general, and other special hospitals. Other special hospitals include obstetrics and gynecology; eye, ear, nose, and throat; rehabilitation; orthopedic; and other individually described specialty services. Community hospitals may include academic medical centers or other teaching hospitals, if they are nonfederal short-term hospitals. Excluded are hospitals not accessible to the general public, such as prison hospitals or college infirmaries.
- Systems
- System is defined by AHA as either a multihospital or a diversified single hospital system. A multihospital system is two or more hospitals owned, leased, sponsored, or contract managed by a central organization. Single, freestanding hospitals may be categorized as a system by bringing into membership three or more, and at least 25 percent, of their owned or leased nonhospital pre-acute or post-acute health care organizations. System affiliation does not preclude network participation.
- Network
- Network—or vertically integrated healthcare network—is a group of hospitals, physicians, other providers, insurers and/or community agencies that work together to coordinate and deliver a broad spectrum of services to their community. Network participation does not preclude system affiliation. A vertically integrated healthcare network combines (a) facilities, (b) physicians – who are on salary to or under contract to the network – and (c) insurance plans*, all under a single corporate entity. [Consult the pdf document entitled "2012 Top 100 IHNs"—Integrated Healthcare Networks.]
Given our current focus on "public" facilities and public health administration, you should note that approximately one facility in every five is government owned and/or managed, while the remaining 80% are privately owned and managed. A majority of these facilities are small, rural, county-owned hospitals. In the State of Idaho, for example, approximately one half of all hospitals are county-owned.
Note that there are three sides to the Public Health Administration diagram (triangle):
- Health Policy and Administration
- Health Education and Behavior
- Epidemiology
Health Policy and Administration has two principal components: (1) to develop and administer health policies, and (2) to manage healthcare provider organizations, such as military hospitals and clinics, state mental hospitals, Veterans Administration Hospitals, etc.
Health Education and Behavior is dedicated to the development and implementation of educational programs to promote health and reduce, prevent or eliminate disease. This is comprised of a combination of national as well as state and local initiatives. These initiatives have touched each of our lives in many ways, from immunizations to school health nurses, to state and regional programs.
Epidemiology is dedicated to the application of statistical measures to study disease patterns and to help us control the spread of infectious or communicable diseases. The Centers for Disease Control and Prevention are federally funded organizations that lead epidemiological initiatives. [Note: Inasmuch as you are going to be pursuing a career in the healthcare industry, we strongly suggest that you take a course in epidemiology.]
As you continue your Healthcare Administration studies, you should know that there is an undergraduate major in Public Health Administration. It is a companion major to Healthcare Administration—which is the discipline of learning to manage non-governmental, private, provider organizations, e.g., acute-care hospitals, ambulatory surgery centers, long-term care facilities, rehabilitation facilities, medical group practices and hospice and palliative care organizations. One of the major purposes of this introductory course is to introduce you to these six types of provider organizations and to give you enough information to help you begin to envision an array of possible priorities from which you may choose your career focus.
[CDC] Centers for Disease Control and Prevention
Healthcare Industry Sector 2: The Private Sector
The "private" or non-government sector of the healthcare industry is comprised of six types of healthcare provider organizations:
- Acute-care Hospitals
- Ambulatory Surgery Centers
- Physician clinics or medical group practices and Urgent Care clinics, which are a subtype of Medical Group Practice
- Inpatient and/or Outpatient Rehabilitation Facilities
- Long-Term Care Facilities
- Hospice and Palliative Care Organizations, including Home Health agencies.
Note: Do not confuse the various types of "provider organizations" with the following five working components of the industry and how it functions. The provider organizations listed above all comprise "Providers" in the healthcare industry.
The Healthcare Industry structure, at its most basic level, is comprised of the following components:
Patients
All health care is designed to provide services to patients – individuals who are physically ill, injured, psychologically or emotionally ill, or who have need of assistance with "activities of daily living. [ADLs]."
Providers
Acute Care Segment vs Long-term care segment:
- Acute Care is the segment of the industry that treats (delivers services to) patients who are injured or ill. (Psychiatric care is often considered part of acute care.) It is designed to diagnose, treat, and cure or ameliorate (improve the health status) of patients who desire to return, as much as possible, to normal daily function. "Palliative care (from Latin palliare, to cloak) is an area of healthcare that focuses on relieving and preventing the suffering of patients. Unlike hospice care, palliative medicine (pain and symptom relief) is appropriate for patients in all disease stages, including those undergoing treatment for curable illnesses and those living with chronic diseases, as well as patients who are nearing the end of life. Palliative medicine utilizes a multidisciplinary approach to patient care, relying on input from physicians, pharmacists, nurses, chaplains, social workers, psychologists, and other allied health professionals in formulating a plan of care to relieve suffering in all areas of a patient's life. This multidisciplinary approach allows the palliative care team to address physical, emotional, spiritual, and social concerns that arise with advanced illness." (Wikipedia)
- Long-term Care is the segment of the industry that treats (delivers services to) patients who need assistance with Activities of Daily Living [ADLs]. Long-term care patients are generally the elderly, the disabled, or those who cannot function optimally by themselves. We have traditionally referred to this segment of the industry with a generic term: "Nursing Home."
Activities of Daily Living
Basic ADLs consist of self-care tasks, including
- Personal hygiene and grooming
- Dressing and undressing
- Self feeding
- Functional transfers—getting from bed to wheelchair, getting onto or off of the toilet, etc.
- Bowel and bladder management
- Ambulation (walking or "getting around")
Instrumental Activities of Daily Living
Instrumental Activities of Daily Living are not necessary for fundamental functioning, but they permit an individual to live independently in a community, i.e., not being institutionalized:
- Housework
- Taking Medications as prescribed
- Managing money
- Shopping for groceries, clothing or necessities
- Use of telephone or other forms of communication
- Using technology (as applicable)
- Transportation within the community
There are numerous "home health” agencies whose business it is to deliver these services.
You should be able to distinguish between the acute care segment of the industry, the purpose of which is to "diagnose, treat, cure (or ameliorate) and then return the patient to his/her normal daily routine, and the long-term care segment (which we have traditionally referred to as "nursing homes”). Its purpose is to assist individuals with activities of daily living and to assist in the management or treatment of "chronic" conditions (from which there is no cure).
Healthcare Provider Organizations – facilities that comprise the acute-care and long-term care segments of the industry
Healthcare Provider Organizations—facilities that comprise the
acute-care and long-term
care segments of the industry
Acute-care Organizations:
- Hospitals
- Ambulatory Surgery Centers
- Urgent Care Clinics and/or Retail Health Clinics
- Medical Group Practices
Long-Term care Organizations:
- The Patient’s Home [Home Health]
- Assisted Living Centers
- Nursing Homes
- Skilled Nursing Facilities
Other Healthcare Provider Organizations:
- Rehabilitation Facilities (including
post-acute-care rehabilitation): These facilities deserve special
attention, first because they are often physically connected or
adjoining long-term care facilities; second, because they occupy an
unusual place in CMS reimbursement*; and third, because they
overlap, both acute care and long-term care.
*Reimbursement: Medicare does not reimburse for long-term care. They do, however, pay for one hundred days of acute care and post-acute-care rehabilitation for each "incident” in which a Medicare-eligible patient requires acute care, followed by in-patient or outpatient rehabilitation.
Example: A senior citizen living in a long-term-care facility falls and breaks a hip. He/she is taken by ambulance from the long-term-care facility for surgery at an acute-care hospital. Following the surgery, the patient remains in the hospital for a period of four or five days for post-operative care, which may include physical therapy. Upon orders from his/her physician, the patient is then transferred to a post-acute-care rehabilitation facility. From the beginning of this "incident,” through up to one hundred days (combination of acute care and post-acute-care rehabilitation), Medicare reimburses (a) the ambulance service, (b) the hospital, (c) the physicians involved in the surgery, the anesthesia, the imaging services, (d) a second ambulance trip (if necessary) from the hospital to the rehabilitation facility, and (e) the rehabilitation services prescribed by the attending physician. Regardless of the status of the patient, Medicare discontinues payment on the 100th day of this incident. Note: While this example focuses on a surgical patient, it could just as well have been a senior citizen who develops pneumonia or any other "medical” condition requiring acute care, followed by rehabilitation services.
- Hospice and Palliative Care: Hospice providers are licensed, just like any other healthcare service provider organization. They are unique, however, because they go wherever they are needed in the spectrum of care in the healthcare industry. Much of hospice care is delivered in the patient’s home. It may be delivered in an acute-care hospital. It may also be delivered in any level of longterm care. Hospice is traditionally an option for people whose life expectancy is six months or less, and involves palliative care (pain and symptom relief) rather than ongoing curative measures, enabling a patient to live his/her last days to the fullest, with purpose, dignity, grace, and support. While some hospitals, nursing homes, and other health care facilities provide hospice care onsite, in most cases hospice is provided in the patient’s own home.
For-Profit vs Not-for-Profit Healthcare Organizations (alternative business models)
At the time a business entity is licensed, it is required to declare whether it will function in a For-Profit or a Not-for-Profit business model. Each state is empowered to grant "tax exempt status” to entities that qualify to be not-for-profit. Most had their origins in religious organizations – Catholic, Baptist, Seventh-day Adventist, etc. – that had a strong humanitarian service mission. For now, it suffices to say that there are essentially two differences between for-profit and not-for-profit models:
- For-profit organizations pay taxes (federal, state, and local, where applicable) and they also pay dividends to their shareholders.
- Not-for-profit organizations are exempt from paying taxes and they have no shareholders/stockholders, so they also do not pay dividends.
Please note two important concepts:
- Not-for-Profit hospitals are also known as "voluntary” and For-Profit hospitals are also known as "proprietary.”
- Advocacy (political and legal representation): Not-for-Profit
Hospitals are represented by the American Hospital Association [AHA].
For-Profit Hospitals are represented by the Federation of American
Hospitals [FAH].
"Advocacy" = Latin "vocare” to speak; "ad” to, or on behalf of
To speak on behalf of... To represent the interests of...
Advocacy is legal and/or political representation. The member
organizations of both the FAH and the AHA pay dues. In return, these
advocacy organizations hire or contract for services provided by
lobbyists and lawyers and other staff to represent or influence the
policies, the legislation and/or the issues that are important to their
respective members.
Other advocacy organizations:
- The American Medical Association [AMA] represents physicians**
Note
Some confusion exists in the industry (and the public's perception of the industry) about why the AMA supports or does not support certain issues, such as the Patient Protection and Affordable Care Act of 2010—"ObamaCare." You should be aware that only approximately 30% of physicians are members of the AMA. The other 70% have elected not to become members. The AMA tends to be a very politically liberal organization. By and large, physicians in the U.S. are more politically and socially conservative than the AMA.
- American Nursing Association [ANA]
- The Ambulatory Surgery Center Association [ASCA]
- American Healthcare Association [AHCA] "advocating quality in long-term care”
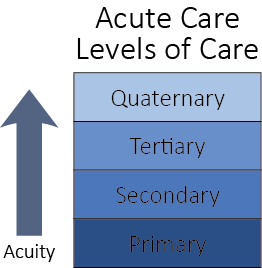
Types of Provider Organizations and the Levels of Acuity of Care Provided Therein
As a precursor to categorizing the types of provider organizations, it is useful to focus on the "levels of care" that typify the organizations and the "acuity" (seriousness of illness or injury) of the services that they deliver. We will then classify the "types" of organizations as they "fit" into those two segments of the healthcare industry.
Acute Care Segment
The acute care segment of the industry is divided into four distinct levels of care, based on the acuity of the illness or injury that will be treated:
- Primary Care: The lowest level of acute care, characterized by the services rendered in physician offices by Family Practitioners, General Practitioners, Pediatricians,Obstetricians and ENTs. It is the "portal" or gateway into the healthcare system and, as such, may include the Emergency Room of a Hospital, a Clinic, an Urgent Care facility, etc.
- Secondary Care: One step/level above "primary"care. All surgery, whether performed in a hospital Operating Room or in an Ambulatory Surgery Center, is at least secondary in acuity, with the exception of minor procedures performed in the physician’s office. ENT physicians, when performing surgery, are delivering secondary care. Obstetrician/Gynecologists, when performing surgery, are delivering secondary care. Any patient who is admitted to a hospital as an in-patient (admitted to a licensed in-patient bed) is receiving at least secondary care. This is the usual and customary level of care delivered in a hospital or ambulatory surgery center.
- Tertiary Care: This term describes treatment for an advanced level of acuity that is generally delivered in an "intensive" care unit or a "special" care unit. Generally, it involves at least one-on-one nursing care. Often there is much more staff involved than that. ICUs are capable of delivering the highest level of care in the acute care setting. Many secondary hospitals have one or more Intensive Care Units for high acuity patients. They may start with a general "med/surg" (combination of internal medicine and post-surgical patients) ICU. As a hospital grows in acuity and adds services, it may have a Cardiac ICU for treatment of heart attack and related issues. It may have a Thoracic ICU for the post-surgical treatment of open heart patients. As a hospital becomes more advanced in Trauma care, it may add a Shock/Trauma ICU. If it requires advanced care for infants, it may add a Pediatric ICU or a Neo-natal ICU. As you can see, tertiary care is an advanced level of care delivered in a hospital that is mostly "secondary" in its usual and customary clinical care.
- Quaternary Care: This level of care is reserved for teaching hospitals, research hospitals and those that are involved with clinical research protocols. Quaternary Care is involved in treatment that is not yet approved by the FDA (U.S. Food and Drug Administration) for day-to-day medical staff privileges. In each institution in which it is delivered, therefore, there is an Institutional Review Board [IRB] that has fiduciary responsibility for overseeing the propriety of the "research” care that is being delivered or proposed. This body is empowered to grant "privileges” to qualified physicians and researchers for a limited or proscribed number of patients (or procedures). These individuals are then required to return and report their findings, their successes and/or failures, to the IRB. Only after a research protocol/procedure is approved by the IRB for day-to-day clinical practice is it included in the catalog of "approved” procedures for non-research physicians to begin providing. It must be added to their medical staff privileges by action of the hospital’s governing board, which has ultimate authority for the quality of care delivered in the institution.
The role of the U.S. Food and Drug Administration (FDA)
In the United States, the Food and Drug Administration has the
responsibility to protect the health and wellness of every citizen.
Every clinical practice, every pharmaceutical medication, every medical
procedure that is practiced upon human patients, must be approved by the
FDA. There is an important relationship between this stewardship of the
FDA and the levels of acute care, which we are describing here. Before
any medical procedure can become part of a physician’s medical staff
privileges, it must have been approved by the FDA. For quaternary
hospitals only, there are provisions for performing "experimental,” i.e.
not-yet-approved for general use by the FDA, procedures, including new
drug protocols. These procedures require clinicians to make application
to the Institutional Review Board of the medical center for temporary
and conditional permission to perform "experimental” procedures on human
patients. As the results of these clinical trials are reported and
documented, the FDA exercises
its fiduciary role and either approves them for use on human patients,
or denies them – in which case they may not be used on human patients.
As they are FDA approved, they are included in the medical staff
privileges of appropriately trained physicians and clinicians.
Having outlined the "Levels of Care” within the Acute Care Segment of the healthcare industry, we are now prepared to focus on the "types” of provider organizations that comprise the acute-care segment, which is separate and distinct from the long-term care segment.
Primary Care
Primary Care is delivered in the following types of Provider Organizations:
- Physician Offices
- Medical Group Practices
- Single specialty (all practitioners have been trained in the same specialty)
- Multi-specialty (include two or more clinical specialties under a single management entity)
- Clinics (primary care)
- Hospital Emergency Rooms/Departments* It is important to note that an ER receives patients ranging in all levels of acuity. They, therefore, perform "triage," which is the procedure by which they assess patient acuity. Generally, patients with a higher level of acuity are given priority, i.e. they are treated first. The ER is considered one of the primary care portals into the healthcare industry. Note that "triage" implies the separation of patients into "three” distinct levels of acuity—not four. That is because quaternary care is not delivered in Emergency Rooms or Emergency Departments.
- Urgent Care Clinics
- Retail Health Clinics
Secondary Care
Secondary Care is delivered in the following types of Provider Organizations:
- Hospitals
- Ambulatory Surgery Centers
- Licensed Recovery Centers*
All provider organizations are licensed by the state in which they operate. All clinical professionals are also licensed by the state in which they operate. The state license identifies the number of licensed in-patient beds (those to which a patient may be admitted when their length-of-stay is longer than twenty-three hours). Ambulatory Surgery Centers are NOT licensed to provide in-patient care. Some ASCs build and operate licensed Recovery Centers (like the Idaho Falls Recovery Center adjacent to the Idaho Falls Surgery Center.) An outpatient (ambulatory) surgery patient, who requires care for longer than 23 hours, may be legally transferred (admitted) to either a licensed Recovery Center or to a full-service hospital. ASCs are required to have a formal transfer agreement for such patients with a nearby full-service hospital, so that patients who require care beyond the level provided at the ASC, or who require care beyond the 23 hours permitted by law, may be transferred to the full-service hospital for care in a licensed inpatient bed.
Tertiary Care is delivered in hospitals that are specifically licensed to provide Intensive Care Services in addition to their secondary care services. The type of ICU (Intensive Care Unit) that is offered is controlled by the state in which the hospital is licensed. A hospital may NOT decide unilaterally, without state approval, that it will provide Intensive Care Services.
Types of Intensive Care Units:
- Medical/Surgical (Med/Surg) ICU
- Free-standing Medical or Surgical ICU
- Pediatric ICU (PICU)
- Neonatal ICU (NICU)
- Coronary Care Unit (CCU)
- Thoracic ICU (for post-operative thoracic surgery patients)
- Shock/Trauma ICU (generally provided in conjunction with a designated Trauma Program, which is licensed according to guidelines established by the American College of Surgeons.)
Note: Some hospitals that are licensed to perform organ transplants are equipped with special ICUs for those patients—liver, kidney, heart, heart-lung, etc.
"Triage" is a term used to describe the assessment of patient acuity (seriousness of injury or illness). At the root of the word is "tri"—three. When patients are separated (triaged), they are divided into (1) primary, (2) secondary, or (3) tertiary levels of acuity. Tertiary patients receive priority care/attention over secondary patients, and secondary patients receive priority care over primary patients. Note that "quaternary" care is not part of this system. It is reserved for research protocols that are the domain of teaching hospitals with a research mission.
Quaternary Care is the exclusive domain of Teaching/Research Medical Centers. It is research oriented. Whenever a new treatment of any kind is offered, it must first be presented to an Institutional Review Board of the hospital or medical center where the research is proposed. The IRB may approve or deny the proposed research protocol. If it is approved, it must be carried out under strict supervision of the IRB.*
Payers
The third component of the healthcare industry (we have previously
discussed both "Patients" and "Providers") is the group we know as the
payers for healthcare services. The Healthcare Industry is unique in
this regard, because in no other industry does the "buyer” (patient) not
have the direct responsibility to pay for the goods or services that
he/she uses. The term "thirdparty payer” is a very unusual thing, but it
is the norm in this industry.
There are essentially three major Payers in the Healthcare Industry:
- The Patient, i.e., "Private Pay."
- The Government through CMS—Centers for Medicare and
Medicaid Services
- Federal: Medicare—those 65 years of age or older, and the disabled
- State: Medicaid—those who are "indigent," i.e., living below the federal poverty line (FPL)
- Traditional Health Insurance Companies, who offer
two types of Insurance Plans:
- Indemnity Plans: Blue Cross, Blue Shield, Aetna, DMBA, etc.
- Managed Care Plans: HMO or PPO, etc. "Guaranteed coverage for a fixed annual premium. (We will cover insurance plans in greater depth later in these materials.)
Note: With the enactment of the Affordable Care Act of 2010, new forms of insurance plans are emerging, e.g. Accountable Care Organizations, which are designed to encourage greater commitment to preventative care and which significantly alter the traditional methods of reimbursement.
The relative percentage of all payments for healthcare services:
- Government: >50%
- Traditional Insurance + Managed Care: >40%
- Private Pay Patients: 6%–8%
There are two remaining components in the structure of the healthcare industry:
Provider Organizations and Ownership Status
There are three different ownership models into which healthcare provider organizations are divided:
- Free-standing facilities – institutions who stand alone and whose operating profits/losses accrue only to themselves.
- Facilities that are part of a "chain" or multi-hospital system, e.g., Hospital Corporation of America
- Facilities that are part of Vertically Integrated Healthcare Networks [IHNs] like Intermountain Healthcare. IHNs are a type (subgroup) of multi-hospital systems. However, they contain two components that not all "systems" contain:
- They "own" and/or "have under contract" physicians and
- They own their own health insurance companies
All Integrated Healthcare Networks are Multi-Hospital Systems. Not all Multi-Hospital Systems are IHNs. If they lack (do not own) their own health insurance company, they cannot qualify as an IHN.
Hospital Corporation of America [HCA] owns facilities and physicians. It does not own a healthcare insurance company – it is a multi-hospital system.
Intermountain Healthcare [IHC] owns facilities, physicians and a
healthcare insurance company—it is both a multi-hospital system and an
Integrated Healthcare Network.